Understanding Double Vision (Diplopia)
Double Vision (Diplopia): What It Is and Why It Happens
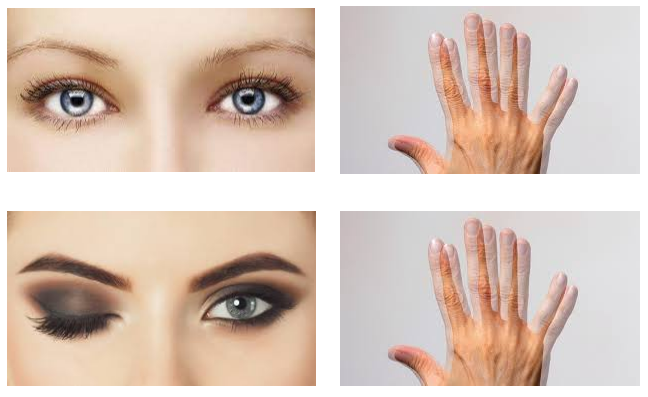
Seeing double can be alarming, especially when it appears suddenly or interferes with everyday tasks such as reading, walking, or driving. Clinically referred to as diplopia, double vision occurs when a single object is perceived as two images instead of one. These images may appear side by side, one above the other, or slightly offset at an angle.
For some people, the second image looks faint or shadow-like, often described as a “ghost image.” Because of this, diplopia is frequently mistaken for blurred vision. However, while blurred vision produces one unclear image, diplopia involves two separate visual perceptions that the brain cannot merge correctly.
Diplopia can be temporary and benign, but it can also point to underlying eye, nerve, muscle, or neurological issues. Understanding what double vision looks like and how it presents is an important first step in knowing when professional assessment is needed.
What Does Double Vision Look Like?
Double vision does not look the same for everyone. Common real-world experiences include:
Letters appear doubled or overlapping when reading
Two road signs or traffic lights appear instead of one
Objects appear misaligned, particularly when looking into the distance
Difficulty judging steps, curbs, or hand placement
Symptoms improve or disappear when one eye is closed
These visual disruptions might greatly affect balance, depth perception, and coordination, which is why diplopia usually feels more disabling than simple blur.
What Is Diplopia?
Diplopia is a symptom, not a diagnosis. It describes the brain receiving two visual signals instead of one unified image. This can occur because of issues within one eye or because both eyes are no longer working together properly.
Clinically, diplopia is classified into two main types:
Monocular diplopia
Binocular diplopia
Distinguishing between these two forms is one of the most important steps in identifying the underlying cause.
Monocular Diplopia (Double Vision in One Eye)
Monocular diplopia persists even when the unaffected eye is closed. This means the doubling originates within a single eye rather than from eye coordination problems.
Common causes include:
Astigmatism
Cataracts
Dry eye disease
Irregularities of the cornea
Ill-fitting glasses or contact lenses
Because monocular diplopia is usually optical in origin, it is less commonly linked to neurological conditions. However, persistent monocular double vision still requires assessment, particularly if symptoms worsen or disturb daily activities.
Binocular Diplopia (Double Vision in Both Eyes)
Binocular diplopia occurs only when both eyes are open and resolves when either eye is closed. This form of double vision is caused by misalignment of the eyes, meaning each eye is pointing at a slightly different target.
Potential causes include:
Eye muscle imbalance
Nerve damage affecting eye movement
Thyroid eye disease
Diabetes-related nerve changes
Neurological conditions affecting coordination
Because binocular diplopia can be associated with more serious underlying conditions, it is often treated with greater urgency than monocular diplopia.
Horizontal, Vertical, and Diagonal Double Vision
Horizontal Double Vision
Images appear side by side. This is commonly linked to issues with the muscles responsible for moving the eyes left and right. People often notice horizontal diplopia more when looking into the distance or when fatigued.
Vertical Double Vision
One image appears above the other. This type can feel particularly disorienting when walking or using stairs and may be associated with vertical eye muscle dysfunction.
Diagonal Double Vision
Images are separated both horizontally and vertically. This pattern may indicate more complex alignment or neurological involvement.
Each presentation yields valuable diagnostic information during an eye examination.
Common Causes of Double Vision
Double vision can arise from problems affecting different parts of the visual system. Understanding the category of cause helps guide appropriate investigation and management.
Optical Causes (Within the Eye)
These typically result in monocular diplopia and include:
Uncorrected refractive errors
Cataracts
Corneal surface irregularities
Severe dry eye
Eye Muscle and Alignment Causes
These usually lead to binocular diplopia and may include:
Strabismus (eye turn)
Muscle weakness or restriction
Injury affecting eye movement
Neurological Causes
Some cases of diplopia originate from nerve or brain involvement, such as:
Cranial nerve palsies
Stroke or transient ischaemic attack
Multiple sclerosis
Brain tumours or aneurysms
Head trauma
Sudden-onset double vision without an obvious cause should always be assessed promptly, as it can be a neurological warning sign.
Systemic Health Conditions
Certain medical conditions can interfere with eye movement control, including:
Diabetes
Thyroid disorders
Myasthenia gravis
Systemic health and vision are closely linked, which is why a full health history is an important part of diplopia assessment.
When Is Double Vision a Medical Emergency?
Double vision should never be ignored, particularly if it appears suddenly.
Seek urgent medical attention if:
Double vision develops suddenly without explanation
It follows a head or facial injury
It occurs alongside headache, weakness, dizziness, or speech difficulty
There is eyelid drooping or facial asymmetry
Arrange an eye examination if:
Double vision is persistent or worsening
It interferes with reading, driving, or balance
It is associated with eye pain or redness
Early assessment allows serious causes to be ruled out and proper management to begin.
How Double Vision Is Diagnosed
Diagnosing diplopia includes determining whether the cause is optical, muscular, neurological, or systemic.
Comprehensive Eye Examination
An eye examination typically includes:
Visual acuity testing
Assessment of eye alignment and movement
Refraction to check focusing errors
Evaluation of eye health structures
This step often identifies whether the diplopia is monocular or binocular and helps narrow down potential causes.
Neurological Assessment
If eye findings show nerve involvement, further neurological evaluation may be recommended. This can help identify conditions affecting coordination, muscle strength, or nerve signalling.
Imaging Tests (MRI or CT scan)
Imaging tests such as Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans may be recommended when double vision raises concern about possible involvement of the brain, nerves, or surrounding structures. These scans provide precise images that help clinicians identify or rule out conditions affecting the routes responsible for eye movement and visual processing.
Imaging is not routinely required for every case of diplopia. Instead, it is typically considered when double vision appears suddenly, is unexplained, is associated with neurological symptoms, or follows head trauma. The decision to proceed with imaging is based on findings from the eye examination, symptom history, and overall clinical assessment.
By using imaging selectively rather than routinely, medical professionals can focus investigations where they are most likely to be informative, while preventing unnecessary testing in cases where the cause of double vision is clearly optical or muscular in origin.
Treatment Options for Diplopia
Treatment depends entirely on the underlying cause and may change over time as the condition stabilises or improves.
Optical Correction
Updated glasses or contact lenses
Prism lenses to help realign visual images
Prisms do not correct the cause but can considerably reduce symptoms in suitable cases.
Temporary Symptom Management
Short-term eye patching
Temporary prisms during recovery phases
These measures may be used while the underlying condition is healing or stabilising.
Medical Management
When diplopia is linked to systemic or neurological conditions, treatment may involve:
Managing blood sugar levels
Addressing thyroid dysfunction
Medications for neuromuscular conditions, where appropriate
Surgical Options
In selected cases where eye alignment does not improve, eye muscle surgery may be considered. Surgery is typically delayed until the condition has stabilised to maintain long-term effectiveness.
Living With Double Vision
Visual Adjustments
Improving lighting for reading and close work
Reducing screen glare and eye strain
Using larger text where possible
Daily Activity Modifications
Taking regular breaks during visually demanding tasks
Avoiding driving until cleared by a professional
Using handrails or supports if depth perception is affected
Emotional and Psychological Impact
Living with persistent double vision can be frustrating and emotionally challenging. Feelings of anxiety or reduced confidence are common, particularly when independence is affected. Support from healthcare professionals and, where needed, counselling services can help individuals adapt while treatment is ongoing.
Preventing Vision Problems That Lead to Diplopia
While not all causes of diplopia are preventable, general eye health measures can reduce risk:
Regular eye examinations
Prompt management of systemic health conditions
Protective eyewear during high-risk activities
Early assessment of any new or unusual visual symptoms
Frequently Asked Questions
Is diplopia always serious?
Not always, but it should always be assessed to rule out serious causes.
Can double vision go away on its own?
Yes, particularly if related to fatigue or temporary nerve inflammation. Ongoing symptoms should be reviewed.
Can stress cause double vision?
Stress can worsen eye strain, but it is rarely the sole cause of true diplopia.
Are exercises enough to fix double vision?
Exercises may help in selected cases but should only be done under professional guidance.
Conclusion
Diplopia is a visual symptom that can range from minor optical issues to serious neurological conditions. Understanding what double vision looks like, recognising the difference between monocular and binocular diplopia, and knowing when to seek assessment are important steps in protecting both vision and overall health.
If double vision is persistent, sudden, or interfering with daily life, professional assessment is the safest way to identify the cause and guide appropriate care.